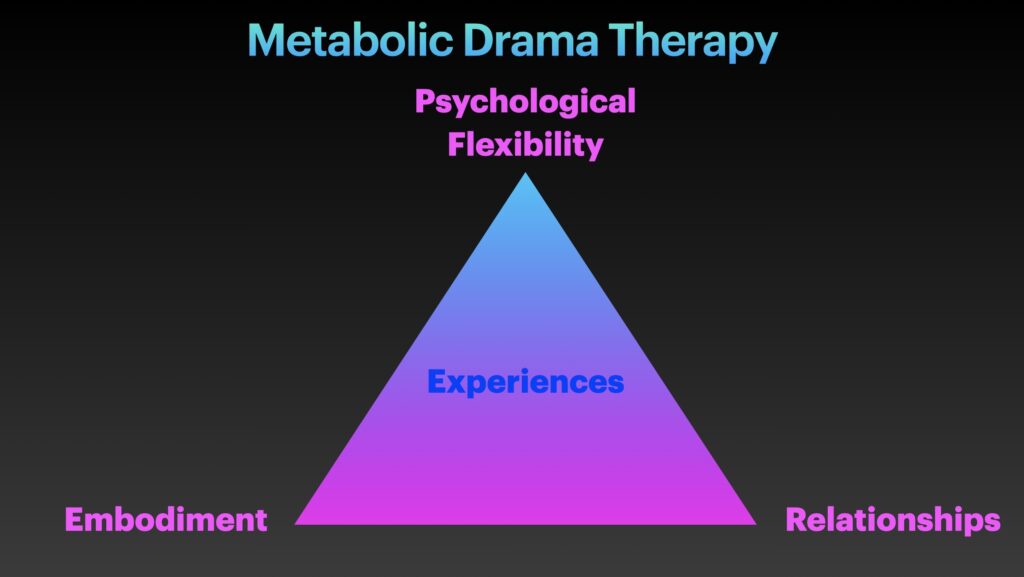
Below is a modified version of my capstone paper for my drama therapy graduate program. My overall project conceptualized drama therapy through a metabolic lens (‘Metabolic Drama Therapy’) and resulted in creation of a card deck of practices intended to support wellness and wellbeing by improving metabolic and mental health through lifestyle, stress reduction, and improved psychological flexibility. First draft of the deck is currently being printed; more details to come! The below paper goes into the underlying theory of the relationship between mental health and metabolic health. Essentially, our physical health impacts our mental health and our mental health impacts our physical health. Mind and body are connected.
The mental health field largely points to a ‘biopsychosocial’ model to explain the complex etiology of mental health issues. There’s genetics, environment, attachment. Reward, punishment, and learning. Neurotransmitters. Inflammation. Hormones. The gut microbiome. Neglect, trauma, abuse, and adverse childhood experiences [ACEs]. Poverty, race, and socioeconomic status. Social isolation. Psychological stress. Temperament and personality, psychological rigidity. Beliefs, schemas, and cognitive distortions. All these factors impact mental health. Indeed, research findings “have demonstrated that psychosocial experiences and life exposures influence subcellular processes including immune activation/suppression, oncogenic behavior, gene expression regulation, telomere maintenance, and epigenetic processes” (Picard & McEwen, 2018b, p. 142). Our emotional experiences, regardless of valence, are “suspected to trigger broad-acting biological pathways such as inflammation that meaningfully influence morbidity and mortality” (Picard & McEwen, 2018b, p. 142).
Research is increasingly converging on the role of mitochondria in mediating these processes in mental health both as targets of stress and mediators of stress pathophysiology (Picard & McEwen, 2018b). It is worth noting much of the research on stress and mitochondria has been conducted with male animals (Zitkovsky, Daniels, & Tyrka, 2021). In addition to potential differences between animal and human physiology and impacts of age, it is also important to consider biological sex differences as “both mitochondria and neuroendocrine pathways are sensitive to sex hormones” (Zitkovsky, Daniels, & Tyrka, 2021, p. 7).
Some people may be familiar with the notion of mitochondria as the ‘powerhouse’ of the cell. More than just an energy producing organelle, the mitochondrion “represents a critical nexus of biological, psychological, and social factors that underlie the mechanisms and consequences of the stress response. Psychosocial factors impact biological processes through physiological systems that are highly integrated with mitochondrial functioning” (Daniels, Olsen, & Tyrka, 2020, p. 2). Because the brain is so highly populated with mitochondria, “there is profound impact of mitochondrial dysfunction on psychological processes, with increasing evidence demonstrating associations of stress-related mitochondrial dysfunction and psychopathology” (Daniels, Olsen, & Tyrka, 2020, p. 2). Describing the role of mitochondria in the detail it deserves is beyond the scope of this paper. Please see Daniels, Olsen, & Tyrka (2020) for an excellent review and orientation to the role of mitochondria in psychological stress.
Conceptualizing mental health issues as metabolic dysregulation opens up metabolic treatments and de-mystifies how various processes and experiences impact mental health and wellbeing. ACEs set children up for a lifetime of poor health including substance abuse disorders, obesity, cardiovascular disease, increased risk of cancer, higher all-cause mortality (Zitkovsky, Daniels, & Tyrka, 2021). ACEs are also associated with psychiatric disorders, pointing to the overlap between metabolic health and mental health (Zitkovsky, Daniels, & Tyrka, 2021). According to Zitkovsky, Daniels, & Tyrka (2021) “severe stress and associated alterations in glucocorticoid signaling promote mitochondrial dysfunction through altering mitochondrial dynamics” (p. 6). Early life adversity may exert a physiological effect through mitochondria that ultimately affects the entire biological system (Zitkovsky, Daniels, & Tyrka, 2021).
Research has shown trauma can be inherited in humans (Bowers & Yehuda, 2016; Yousef et al., 2018). This process is thought to be mediated by epigenetics. The epigenome “can accommodate environmental influences in the form of chemical and protein modifications of chromatin (consisting of DNA, protein, and RNA). Epigenetic changes can be long lasting and alter gene regulation and expression” (Daskalakis et al., 2018, p. 2). Exposure to psychological trauma is a strong risk factor for mental disorders and affects biology in these individuals (Youssef et al., 2018). This further points to a common mechanism underlying physical and mental disorders. Youssef et al. (2018) note many of the studies in their review found the gene for the glucocorticoid receptor was associated with inherited epigenetic changes: “maternal exposure to war violence or rape during pregnancy was associated with increased methylation in the…promoter region [for the glucocorticoid receptor gene] in newborns” (p. 5). Glucocortioids are stress hormones (Youssef et al., 2018). Stress can adversely affect mitochondrial function. Trauma, whether it is inherited or directly experienced by an individual, may ultimately exert its harmful effects through damaging mitochondrial function.
Picard & McEwen (2018b) reviewed 23 studies (all of which used male animals) looking at the impact of psychological stress on mitochondrial function. Picard & McEwen (2018b) conclude “overall, evidence supports the notion that acute and chronic stressors influence various aspects of mitochondrial biology, and that chronic stress exposure can lead to molecular and functional recalibrations among mitochondria” (p. 141). More comprehensive research is needed in humans taking into account effects of biological sex, age, type of stress, duration, stressor intensity, individualized emotional response, and other variables (Picard & McEwen, 2018b).
In their 2020 systematic review and meta-analysis, Shields, Spahr, & Slavich looked at 56 unique randomized clinical trials with a total of 4,060 participants to see the impact of psychosocial interventions on the immune system. They found “psychosocial interventions were associated with positive changes in immunity over time, including improvements in beneficial immune system function and decreases in harmful immune function” for participants randomly assigned to psychosocial interventions vs control (p. 1). Notably, “these associations were most reliable for cognitive behavior therapy [CBT] and multiple or combined interventions and for studies that assessed proinflammatory cytokines or markers” (Shielfs, Spahr, & Slavich, 2020, p. 1). Psychological interventions can impact physiology in significant and sustained ways. Body and mind are not wholly separate entities.
Conceptualizing mental health and overall wellbeing as fundamentally related to metabolism and mitochondrial health presents opportunities for effective treatments and preventive efforts. Two prominent figures in the emerging field of metabolic psychiatry are Chris Palmer, a psychiatrist at Harvard, and Shebani Sethi Dalai, a psychiatrist at Stanford. I asked Palmer via Twitter if he was aware of any research on metabolic effects of ‘typical’ psychotherapy modalities (like cognitive-behavioral, dialectical behavioral, acceptance and commitment, expressive arts, internal family systems). He responded, “We don’t have much research linking these psychotherapies directly to metabolism/mitochondria, but I support their continued use for many reasons…I believe they help a lot of people, but not everyone. Some people need other treatments” (Palmer, 2022). Palmer is a proponent of ketogenic diets for serious mental health issues like schizophrenia and bipolar, viewing a ketogenic diet as a metabolic intervention. While a deeper exploration on diet and nutrition for mental health is beyond the scope of this paper, it is crucial to note the significant role of sound nutrition in psychological wellbeing.
If mitochondria are at the root not only of physical diseases including aging, cancer, and inflammation but also our psychological wellbeing, then it is essential to engage in practices that support, nurture, and protect mitochondria. The level of intervention required for a given individual likely depends on severity of metabolic dysfunction. An obese person with type 2 diabetes, heart disease, and schizophrenia requires a stronger degree of intervention than someone with mild life stressors and no history of acute trauma exposure. Medication and other medical treatments may be necessary for some individuals.
Aside from nutrition, numerous lifestyle practices influence mental health. These include sleep, exercise/movement, and light exposure (viewing bright light early in the day and avoiding bright light at night). Light exposure affects circadian rhythms, which are strongly associated with mental health (Walker et al., 2020). Circling back to glucocorticoids, “the two most prominent endocrine manifestations of circadian rhythms are the daily cycles of melatonin and glucocorticoids” (Walker et al., 2020, p 4). Cortisol, the so-called ‘stress hormone’, is a glucocorticoid (Walker et al., 2020). Bright light therapy is one of several successful treatments for depression (Walker et al., 2020). A seemingly simple behavior, an action, a practice—like viewing bright light at a certain time of day—can exert a potent effect on mental health.
Conceptualizing mental health issues as metabolic issues moves away from distinct diagnostic categories as delineated in the mental health field’s standard text, the DSM, and towards processes. Despite extensive research, there are no biological markers for mental disorders (Hoffman, Hayes, & Lorscheid, 2021). Any number of biopsychosocial factors can cause metabolic and mitochondrial dysfunction, from genetics and epigenetics to environmental toxins to broader societal dynamics that significantly influence an individual’s biochemistry.
Picard et al. (2018) distinguish different types of stress responses an individual may experience in response to various external events. Notably, “toxic stress” is experienced when an individual experiences an aversive event but “lacks internal resources or external support systems, and, as a result, there is a lack of sense of control that leads to a chronic physiological dysregulation that promotes pathophysiology…Lack of control has been one of the defining features of psychological stress that leads to disease” (Picard et al., 2018, p. 73). It is possible a sense of lack of control is subjective. How one relates to and perceives the stressor—and not necessarily the stressor itself—may have implications for mental and physical health.
Stress, including psychological stress, increases energy demand (Picard et al., 2018). Heart rate and blood pressure have been shown to increase by 10-20% solely due to psychological stress (Picard et al., 2018). Mitochondria are directly involved in cellular energy production. Importantly, “complex stimuli such as social interactions and other stressors are associated with behavioral responses which incur elevation in energy demand, also met by mitochondrial energy transformation…Stress in particular increases cerebral energy demand including oxidation of glucose and oxygen consumption…reflecting increased mitochondria activity within the brain” (Picard et al., 2018, p. 75). Intangible processes such as cognition and social interactions exert real effects on our physiology. The idea of ‘thoughts as energy’ has merit. Many people do not respond to their stressors with physically demanding behaviors such as running or fighting and as a result “stress hormones can dysregulate metabolism” (Picard et al., 2018, p. 77). In humans this translates to “higher circulating levels of cortisol under resting (non-stressed) conditions” and “higher levels of glucose and triglycerides, and a higher score reflecting insulin resistance and a pre-diabetic state” (Picard et al., 2018, p. 77).
An individual cannot undo their past adverse life experiences. We have no control over the events of our parent’s lives and how the impact of those may have been passed on to us, embedded in our physiology. We can and should strive for a more just and equitable society. We can donate within our means to help those less fortunate and participate in social justice causes meaningful to us. And at the same time, conceptualizing our psychological health through the lens of metabolism and mitochondria unlocks powerful tools we can use in the here and now to improve our wellbeing. The central question to ask is, what will benefit my mitochondria and the answers will vary across individuals depending on many varied biopsychosocial factors and context.
We can intervene directly into physiological processes that impact the mitochondria. These include improving sleep, nutrition, light exposure, and physical activity. Mattson et al. (2018) discuss the physiological and biochemical processes underlying how “intermittent metabolic switching” via repetition of cycles of fasting and exercise to induce ketosis followed “by a recovery period (eating, resting, and sleeping) may optimize brain function and resilience throughout the lifespan” (p. 1).
Getting adequate sleep, incorporating physical activity, and eating healthy foods are challenges for many people. Reasons can vary: lack of financial resources, lack of education on healthy diet, beliefs and values (including societal and cultural), food addiction, work demands, time constraints, and stress. Additionally, as discussed previously, our internal world and how we relate to it can impact metabolism. Our experiences, our relationships, our sense of belonging and meaning— these processes matter for overall wellbeing as all impact mitochondrial functioning.
Steven Hayes, creator of Acceptance and Commitment Therapy [ACT] is a proponent of a process-based approach to mental health treatment. Through this lens clinicians “shift their focus to the most important biopsychosocial processes for a given client, given their goals and current circumstances, and to identifying the methods that best move them toward those goals with greater freedom to consider processes and methods across traditions and approaches” (Hoffman, Hayes, & Lorscheid, 2021, p. 7). A process-based approach asks “What core biopsychosocial processes should be targeted with this client given this goal in this situation, and how can they most efficiently and effectively be changed?” (Hoffman, Hayes, & Lorscheid, 2021, p. 7). The answer for a given individual depends on their metabolic context and provides a powerful direction for interventions. It deconstructs disorders like depression and anxiety into various biopsychosocial processes that can be unique for any given person. The processes underlying one person’s anxiety may differ from someone else’s, and the tools to enact change may come not only from different school of psychotherapy but also from practices centered on improving nutrition, sleep, social connections, physical activity, and more.
The domains included in Hayes’s process-based approach are affect, cognition, self, attention, behavior, motivation, biophysiological, context, and sociocultural (Hoffman, Hayes, & Lorscheid, 2021). Each domain includes several mediators such as beliefs, cognitive defusion, mindfulness, self-compassion, spirituality, values, coping skills, dietary intake, exercise, and social support (Hoffman, Hayes, & Lorscheid, 2021). These change processes function together in a system that impacts an individual’s mental and physical health. The 6 core processes targeted in ACT are acceptance, cognitive defusion, presence, self as context, values, and committed action, with an overarching goal to increase an individual’s psychological flexibility (Hayes, n.d.).
Psychological flexibility includes being able to: “recognize and adapt to various situational demands; shift mindsets or behavioral repertoires when these strategies comprise personal or social functioning; maintain balance among important life domains; and be aware, open, and committed to behaviors that are congruent with deeply held values” (Kashdan & Rottenberg, 2010, p. 1). Kashdan & Rottenberg (2010) further note “in many forms of psychopathology, these flexibility processes are absent” (p. 1). Biopsychosocial factors including attachment/family dynamics, socioeconomic status, and religion likely impact and shape an individual’s psychological flexibility (Venkatesh et al., 2021).
Browne et al. (2022) found psychological flexibility mediated wellbeing for an Irish cohort of adults who had experienced ACEs: “psychological flexibility was strongly and significantly associated with decreases in psychological distress and improved wellbeing. It significantly mediated the relationship between ACE and wellbeing” (p. 1). At the time of writing, a search on PubMed for research on ‘psychological flexibility mitochondria’ within the last 10 years returned three results, none of which were relevant. It is therefore simply a hypothesis at this time that changing how we relate to our experiences and moving towards greater psychological flexibility might beneficially impact our physical and mental wellbeing through improving mitochondrial functioning and cellular energetics.
Numerous lifestyle and behavioral intervention points can improve mitochondrial health (in addition to those within medicine which are beyond the scope of this paper). These include diet, sleep, social connection, physical activity, spirituality, beliefs, finding a sense of joy/meaning/purpose, and mindfulness. Many such wellness and wellbeing practices naturally arise from various psychotherapy modalities such as dialectical behavior therapy [DBT], acceptance and commitment therapy [ACT], compassion focused therapy [CFT], internal family systems [IFS], and the action-oriented and embodied approach of drama therapy. Drama therapy integrates all these and more as it involves numerous change processes such as relationship (both to self and others), embodiment, movement, cognition, behavior, mindfulness, creativity, compassion, play, spirituality, and perhaps most importantly, flexibility.
Drama therapy is rooted in flexibility. A core drama therapy process of externalization of internal experience facilitates a more flexible way of relating to it. From an ACT lens, this perhaps falls under the process of ‘cognitive defusion’ although it can be utilized for a variety of non-cognitive internal experiences including feelings, physical sensations, and urges/impulses. It can also facilitate a more flexible way of relating to most anything in an individual’s life, including objects, other people, and stressors via perspective taking. Additionally, engaging in most any drama therapy process can function as behavioral activation as well as allow participants direct experience of engaging in action and impact of doing so on mood and cognition.
Our cognition is influenced by more than our individual minds in isolation. Our gestures, our bodies, our spaces, and other people influence our minds. There is an entire field dedicated to researching the role of the body and external resources in shaping cognition— embodied cognition. Embodied cognition presents the “hypothesis that the brain is not the sole cognitive resource we have available to us to solve problems. Our bodies and their perceptually guided motions through the world do much of the work required to achieve our goals” (Wilson & Golonka, 2013, p. 1). Osypiuk, Thompson, & Wayne (2018) summarize evidence pointing to a “bi-directional relationship between body posture and mental states” and “hypothesize that body posture while standing and/or moving may be a key therapeutic element mediating the influence of [Tai Chi and Qigong] on psychological health” (p. 1).
Neuroscientist Lisa Feldman Barrett’s theory of constructed emotion centralizes the physiological process of interoception at the root of emotion experiences, which we ultimately perceive as concepts learned from the societies and cultures we are embedded in (Barrett, 2017). Our experiences in the world, especially social experiences, shape our minds. Lev Vygotsky, a social psychologist, wrote “through others we become ourselves (Vygotsky, as cited in Bolis & Shilbach, 2018, p. 521). Hegel’s philosophy of dialectics posits “self-consciousness does not emerge through passive individualistic introspection, but through dynamic and reciprocal relations with others” (Bolis & Shilbach, 2018, p. 523).
In their paper on ‘Gesture’s role in speaking, learning, and creating language’ Goldin-Meadow & Alibali (2012) write “there is growing evidence that producing gestures can alter the gesturer’s cognitive state. If this is the case, then a learner’s gestures will not only reflect the process of cognitive change, but also cause that change” (p. 11). Considering the role of movement and the body in cognition, “gesturing does not just reflect thought, but it is part of the cognitive processes that accomplishes a task and, in this sense, is itself thought” (Goldin-Meadow & Alibali, 2012, P. 12).
Similar to externalization in drama therapy, which can function to represent objects/ideas/people/entities that are not present and/or concretize internal experiences, Novack & Goldin-Meadow (2017) discuss gestures may influence cognition “because they are representational actions…they are meaningful substitutions and analogical stand-ins for ideas, objects, actions, relations, etc…Gestures are representational in that they represent something other than themselves, and they are actions in that they involve movements of the body” (pp. 652-653). “
Matheson & Kenett (2020) discuss the role of the motor system in generating creative thought, noting “recent theorizing in embodied or grounded cognition…is relevant for investigating creative thought and building neurocognitive models of creativity. According to this framework, simulations of sensorimotor experience with tools (i.e. information pertaining to tool’s shape, how it feels in the hands, the sounds it makes, and, importantly, the actions it affords) support cognitive processes” (pp. 1-2). Matheson & Kennett (2020) focus on creative/divergent thinking processes utilizing specific tools and note “it may be the case that full bodied embodied simulations support creativity in cases where the tools are less obvious…but the existing evidence does not allow for a strong conclusion as of yet” (p. 4).
While creativity and divergent thinking are often seen as positive traits, skills, or values, there can be a dark side to creativity. This can occur when one’s creative cognitive processes turn to ‘what-if’s’ and anxious worrying, a mind creatively engaged in generating myriad hypothetical worst-case future possibilities. This is where psychological flexibility can be important: hold flexibly to the content of the mind, mindfully choosing what is effective and meaningful in a given context, and what can be let go of. Perhaps this process can support mitochondrial health by dampening the stress response, yielding more energy to devote to effective creative thinking, values-based actions, and engagement with who and what one finds meaningful. Movement, cognition, creativity, indeed all the processes of living, require energy and therefore involve mitochondria.
How we think of and about ourselves is metabolic and can affect our overall health—mental and physical. Not only can thoughts influence overt behaviors as in the CBT model, but they also affect physiology, a process we cannot readily observe (the bi-directional influence of thoughts on physiology is accounted for in the CBT model but is less frequently addressed). The power of thought and belief to effect health outcomes can be so strong that this placebo effect is accounted for in gold-standard research: randomized placebo controlled clinical trials (National Institutes of Health, 2020).
Drama therapy can flexibly integrate effective change processes from other psychotherapy modalities and extend the mind by incorporating the body, space, other people, movement, and objects like scarves and empty chairs. Perhaps certain processes from drama therapy, if regularly engaged with in one’s life, can support mitochondrial health. Mechanism can vary: promoting psychological flexibility, helping people change how they relate to and derive meaning from various internal and external stressors in their lives, promoting meaningful social connections, encouraging action and movement in a largely sedentary culture, helping people cultivate experiences of awe, wonder, play, and positive creativity. These processes all matter. Like all experiences, they influence the physiology of the body. Actions taken or not taken in one’s life have real effects. The self-critical voice, sense of powerlessness, inability to tolerate ambiguity can affect relationships, economic status, and the very core of one’s wellbeing.
References
Alva M. L. (2020). Co-occurrence of diabetes and depression in the U.S. PloS one, 15(6), e0234718. https://doi.org/10.1371/journal.pone.0234718
Barrett, L. F. (2017). How emotions are made. Houghton Mifflin Harcourt.
Bolis, D., Schilbach, L. ‘I Interact Therefore I Am’: The Self as a Historical Product of Dialectical Attunement. Topoi 39, 521–534 (2020). https://doi.org/10.1007/s11245-018-9574-0
Bowers, M. E., & Yehuda, R. (2016). Intergenerational Transmission of Stress in Humans. Neuropsychopharmacology: official publication of the American College of Neuropsychopharmacology, 41(1), 232–244. https://doi.org/10.1038/npp.2015.247
Browne, A., Stafford, O., Berry, A., Murphy, E., Taylor, L. K., Shevlin, M., McHugh, L., Carr, A., & Burke, T. (2022). Psychological Flexibility Mediates Wellbeing for People with Adverse Childhood Experiences during COVID-19. Journal of clinical medicine, 11(2), 377. https://doi.org/10.3390/jcm11020377
Daniels, T. E., Olsen, E. M., & Tyrka, A. R. (2020). Stress and Psychiatric Disorders: The Role of Mitochondria. Annual review of clinical psychology, 16, 165–186. https://doi.org/10.1146/annurev-clinpsy-082719-104030. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8007172/
Daskalakis, N. P., Rijal, C. M., King, C., Huckins, L. M., & Ressler, K. J. (2018). Recent Genetics and Epigenetics Approaches to PTSD. Current psychiatry reports, 20(5), 30. https://doi.org/10.1007/s11920-018-0898-7. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6486832/
Disney, K. (2019, Aug. 6). Motivate children without praise and rewards. Children’s House Montessori of Reston. https://childrenshouse-montessori.com/2019/08/06/motivate-children-without-praise-and-rewards/
Emunah, R. (2020). Acting for real (2nd ed.). New York and London: Routledge.
Goldin-Meadow, S., & Alibali, M. W. (2013). Gesture’s role in speaking, learning, and creating language. Annual review of psychology, 64, 257–283. https://doi.org/10.1146/annurev-psych-113011-143802. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3642279/
Hayes, S. (n.d.). The six core processes of ACT. Association for Contextual Behavior Science. https://contextualscience.org/the_six_core_processes_of_act
Hofmann, S.G., Hayes, S.C., & Lorscheid, D.N. (2021). Learning process-based therapy. Context Press
Kashdan, T. B., & Rottenberg, J. (2010). Psychological flexibility as a fundamental aspect of health. Clinical psychology review, 30(7), 865–878. https://doi.org/10.1016/j.cpr.2010.03.001. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2998793/
Mangurian, C., Schillinger, D., Newcomer, J. W., Vittinghoff, E., Essock, S., Zhu, Z., Dyer, W., Young-Wolff, K. C., & Schmittdiel, J. (2020). Comorbid Diabetes and Severe Mental Illness: Outcomes in an Integrated Health Care Delivery System. Journal of general internal medicine, 35(1), 160–166. https://doi.org/10.1007/s11606-019-05489-3
Matheson, H. E., & Kenett, Y. N. (2020). The role of the motor system in generating creative thoughts. NeuroImage, 213, 116697. https://doi.org/10.1016/j.neuroimage.2020.116697
Mattson, M. P., Moehl, K., Ghena, N., Schmaedick, M., & Cheng, A. (2018). Intermittent metabolic switching, neuroplasticity and brain health. Nature reviews. Neuroscience, 19(2), 63–80. https://doi.org/10.1038/nrn.2017.156. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5913738/
National Institutes of Health. (2020, January). Placebo effect. NIH National Center for Complementary and Integrative Health. https://www.nccih.nih.gov/health/placebo-effect
Novack, M. A., & Goldin-Meadow, S. (2017). Gesture as representational action: A paper about function. Psychonomic bulletin & review, 24(3), 652–665. https://doi.org/10.3758/s13423-016-1145-z
Osborn, D. P., Wright, C. A., Levy, G., King, M. B., Deo, R., & Nazareth, I. (2008). Relative risk of diabetes, dyslipidaemia, hypertension and the metabolic syndrome in people with severe mental illnesses: systematic review and metaanalysis. BMC psychiatry, 8, 84. https://doi.org/10.1186/1471-244X-8-84
Osypiuk, K., Thompson, E., & Wayne, P. M. (2018). Can Tai Chi and Qigong Postures Shape Our Mood? Toward an Embodied Cognition Framework for Mind-Body Research. Frontiers in human neuroscience, 12, 174. https://doi.org/10.3389/fnhum.2018.00174. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5938610/
Palmer, C. [@ChrisPalmerMD]. (2022, Sept. 13). We don’t have much research linking these psychotherapies directly to metabolism/mitochondria, but I support their continued use for many[Tweet]. Twitter. https://twitter.com/chrispalmermd/status/1569895340790226944?s=46&t=1w_5x-2NGY4oVV73ibpI_Q
Perry, B. I., Stochl, J., Upthegrove, R., Zammit, S., Wareham, N., Langenberg, C., Winpenny, E., Dunger, D., Jones, P. B., & Khandaker, G. M. (2021). Longitudinal Trends in Childhood Insulin Levels and Body Mass Index and Associations With Risks of Psychosis and Depression in Young Adults. JAMA psychiatry, 78(4), 416–425. https://doi.org/10.1001/jamapsychiatry.2020.4180
Picard, M., & McEwen, B. S. (2018a). Psychological Stress and Mitochondria: A Conceptual Framework. Psychosomatic medicine, 80(2), 126–140. https://doi.org/10.1097/PSY.0000000000000544
Picard, M., & McEwen, B. S. (2018b). Psychological Stress and Mitochondria: A Systematic Review. Psychosomatic medicine, 80(2), 141–153. https://doi.org/10.1097/PSY.0000000000000545
Picard, M., McEwen, B. S., Epel, E. S., & Sandi, C. (2018). An energetic view of stress: Focus on mitochondria. Frontiers in neuroendocrinology, 49, 72–85. https://doi.org/10.1016/j.yfrne.2018.01.001
Reischer, E. (2016, Feb. 22). Against the sticker chart. The Atlantic. https://www.theatlantic.com/health/archive/2016/02/perils-of-sticker-charts/470160/
Shields, G. S., Spahr, C. M., & Slavich, G. M. (2020). Psychosocial Interventions and Immune System Function: A Systematic Review and Meta-analysis of Randomized Clinical Trials. JAMA psychiatry, 77(10), 1031–1043. https://doi.org/10.1001/jamapsychiatry.2020.0431. Retreived from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7272116/
Venkatesh, S.M., Doan, S.N., Barthel, A.L., & Hofmann, S.G. (2021). Cultural and social influences on individual variation in emotion processes. In S.C. Hayes & S.G. Hofmann (Eds.), Beyond the DSM (pp. 137-163). Context Press.
Walker, W. H., 2nd, Walton, J. C., DeVries, A. C., & Nelson, R. J. (2020). Circadian rhythm disruption and mental health. Translational psychiatry, 10(1), 28. https://doi.org/10.1038/s41398-020-0694-0
Wilson, A. D., & Golonka, S. (2013). Embodied Cognition is Not What you Think it is. Frontiers in psychology, 4, 58. https://doi.org/10.3389/fpsyg.2013.00058
Youssef, N. A., Lockwood, L., Su, S., Hao, G., & Rutten, B. (2018). The Effects of Trauma, with or without PTSD, on the Transgenerational DNA Methylation Alterations in Human Offsprings. Brain sciences, 8(5), 83. https://doi.org/10.3390/brainsci8050083. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5977074/
Zitkovsky, E. K., Daniels, T. E., & Tyrka, A. R. (2021). Mitochondria and early-life adversity. Mitochondrion, 57, 213–221. https://doi.org/10.1016/j.mito.2021.01.005. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8172448/
